Templestowe Day Surgery
Our Mission..., Your optimal Care
Address 2/114 James street, Templestowe VIC. 3106
Ph: 0388223472
Fax: 0388223194
E: templestowedaysurgery@gmail.Com
Services
OUR VISION .. Our Mission

We respectfully acknowledge the Wurundjeri people past and present as traditional owners of the land on which Templestowe Day Surgery is located.
Our Vision:
Our Vision is to be the cosmetic day surgery of choice in the eastern suburbs of Melbourne, recognised as a centre of excellence for both patients and staff. This will be evidenced by measurement and benchmarking of clinical and performance outcomes, patient and staff satisfaction results and safety audit results.
“High profile community Day Surgery For The Times”
Our Mission:
Templestowe Day Surgery aims to enhance the wellbeing of all our clients, bringing comfort and renewed confidence in self, which in turn will open new doors to partake in life’s rich offerings.
This will be achieved through the provision of safe, high quality medical and surgical care which is sensitive to the individual needs and responsive to the situation of each client. The environment at Templestowe Day Surgery is one of warmth, dignity and high quality care that does not discriminate on any basis.
We are community focused and responsive to the evolving needs of this dynamic and important market.
Contact
- Melbourne, Victoria, Australia
MEDICAL ByLAWS

at least one medical practitioner who practises in the field relevant to the clinical scope being reviewed
a 2nd nominee of the relevant professional college, association or society
a nominee medical practitioner chosen by the person who is the subject of the appeal.
- Vision Statement
Our Vision is to be the cosmetic Day Surgery of choice in the eastern suburbs of Melbourne, recognised as a centre of excellence for both patients and staff. This will be evidenced by measurement and benchmarking of clinical and performance outcomes, patient and staff satisfaction results and safety audit results.
It is expected that all credentialed Medical Practitioners will incorporate this vision at all times and in all dealings with and at TDS.
Mission Statement
Templestowe Day Surgery aims to enhance the wellbeing of all our clients, bringing comfort and renewed confidence in self, which in turn will open new doors to partake in life’s rich offerings.
This will be achieved through the provision of safe, high quality medical and surgical care which is sensitive to the individual needs and responsive to the personal situation of each client. The environment at Templestowe Day Surgery is one of warmth, dignity and high quality care that does not discriminate on any basis.
We are community focused and responsive to the evolving needs of this dynamic and important market.
It is expected that all credentialed Medical Practitioners will incorporate this Mission at all times and in all dealings with and at TDS.
Powers and Duties include but are not limited to:
- Delegate such powers, duties and responsibilities to such persons or committees it may deem appropriate from time to time.
- Review and approve credentialing and scope of practice of medical practitioners and specialists applying to use TDS facilities.
- Discuss and make recommendations regarding clinical matters.
- Review and make recommendations regarding new medical equipment and procedures.
- Assess all applications for any new procedures and guidelines in line with current Australian best practice regulations and guidelines.
- The MAC may co-opt additional members as required for advice regarding access, scope of practice and introduction of new equipment and new procedures.
- The MAC may co-opt a consumer representative to be involved in credentialing and scope of clinical practice and service at TDS.
- Review, analyse and make recommendations on clinical incidents and sentinel events.
- Contribute to making and amending By-laws, Rules and Regulations for the management of TDS. The governing body shall carry out annual reviews of such By-laws, Rules and Regulations as required.
- The Governing Body will meet quarterly.
TDS will consider all applications for credentialing to perform Liposuction,Blepharoplasty, Gynecomastia and Skin Treatments procedures. All procedures are to be performed under Local Anesthesia with or without IMI Sedation
- With regards to liposuction the maximum xylocaine dose in tumescent liposuction must not exceed 35mg/kg and the maximum allowable total aspirate (combined total of fat and fluid aspirated) is five (5) litres in a single procedure. Anything exceeding this volume must be undertaken at a different time.
- Liposuction will be performed as per “Guideline for the Providers of Liposuction” Dept of Health Victoria. https://www.health.vic.gov.au/guideline-for-providers-of-liposuction
- With regards to blepharoplasty, gynecomastia and skin treatments these will be performed as per the regulation of Minor Procedures set by the Department of Health https://www.health.vic.gov.au/publications/regulation-of-minor-surgery-in-private-facilities
- Procedures must be performed within the allowed limits of Local Anaesthesia, Methoxyflurane as per https://docs.google.com/document/d/1MSuzOIRXO3HKobfcrT2QaPijwwTVZj3Z/edit and tumescent local anaesthesia as per 2.1. The patient's vital sign must be within normal limits throughout the procedure.
- With regards to IMI sedation. This is administered by the CMP only. The use of Midazolam will be directed by the MAC committee and reviews of the effectiveness will be monitored.
- All other surgical procedures must be performed in accordance with procedural regulations relating to unregistered facilities.
TDS expects that all CMPs will strictly adhere to the Patient Selection for Day Surgery Policy, which details exclusion criteria for admission to TDS, as listed below:
- Age under 18 years
- Weight over 110kg or BMI >/= 35
- Patients assessed by the treating medical practitioner as being of Australian Society of Anaesthetists (ASA) Class 3 or above
- Patients whose surgery is expected to extend beyond two (2) hours duration.
- Patients unable to ambulate without assistance or independently
- Patients with a suspected or confirmed infectious disease of any nature. Patients in question must provide evidence of having met clearance requirements as specified by the National Health and Medical Research Council (NHMRC) guidelines (2019)
- Patients testing positive to active or untreated blood borne viruses (hepatitis B, hepatitis C and HIV)
- Inability or unwillingness to sign or comprehend the required surgical, anaesthetic and financial consent forms (Note: in rare instances a legally authorised guardian or substitute decision maker may be required to help with understanding if the procedure is expected to improve health or wellness outcomes for the patient).
- Absence of a support person to drive the patient home, as deemed necessary by the treating medical practitioner
- History of current obstructive sleep apnoea
- A predisposing diagnosed psychiatric condition unless cleared in advance by the treating psychiatrist
- Known episodes of delirium unless deemed suitable for admission during the surgeons psychological assessment
- Residential address outside Victoria unless confirmed temporary accommodation for at least 3 days post-operatively
- Patients deemed to have a higher than minimal bleeding risk (either medically or due to current medications), as determined by the treating medical practitioner
- Patients who are not amenable to or suitable for outpatient management of pain control
- Anticipated prolonged recovery period for any reason
- Any other reason, as determined by the treating medical practitioner
The following categories of Accreditation for CMPs apply:
- Surgeon
- Surgical Assistant
- Medical practitioner
- Applicants must complete TDS’s Credentialing Application Form and provide:
- Proof of identification
- National and international (if applicable) police check/s
- Original qualifications or certified copies
- Specialist qualification or certified copies
- Procedural qualifications or certified copies
- Current AHPRA registration
- Current medical indemnity insurance that reflects the scope of practice being applied for
- Current CV
- Current CPD evidence
- Two (2) professional referees relevant to the scope of practice being applied for
If the CMP wishes to change to a subset of their current practice – that is, narrowing their scope of practice, they must formally advise the MAC in writing.
A CMP must notify the Medical Director or the Director of Nursing if any conditions have been placed on their medical registration or any other changes to registration or insurance occurs.
All CMPs agree to participate in performance reviews to ensure their competence in the practice that they undertake.
Any notice which is required to be given under any of the By-Laws may be given to a CMP either personally or by sending it by registered mail to him/her at their address as listed on the Accreditation Register. Where a notice is sent by post, the notice shall be deemed to have been received by him/her three days after the date of posting.
Letters of accreditation, signed by the Medical Director or the Director of Nursing on behalf of the Governing Body, shall be issued for a maximum period of three (3) years. Such issue shall be recorded in a register kept for that purpose.
Tenure
- After 3 years, the applicant must complete the TDS re-application for credentialing form.
- The applicant will be presented at MAC and MAC will determine if the applicant is successful.
- Applications for re-appointment are to be directed to the Medical Director
- Applicants will be notified in writing of the outcome of their application.
- Credentialing for Urgent and Temporary Situations
- In the event of an emergency situations in which a current CMP of TDS cannot perform a planned procedure one of the following processes will be undertaken, depending on the circumstances of the case;
- Cancellation or postponement of the planned procedure.
- Transfer of the patient to a suitable registered facility.
- Transfer of the patient via ambulance to an appropriate hospital.
- An accredited CMP who wishes to resign their accreditation status at TDS shall forward a written resignation to the Medical Director of the Governing Body, giving a minimum of 14 days’ notice.
The CMP must at all times observe the highest standards of personal and professional conduct. Without limiting this requirement, the CMP must:
- comply with any reasonable request made by the TDS Medical Director with regard to personal conduct and the provision of services at TDS;
- practice his or her profession in accordance with all applicable codes of conduct, policies, procedures and protocols established by TDS and relevant professional bodies from time to time
- Qualification of a surgeon as a specialist and sub-specialist carries the implication that practice will be conducted within sub-specialty limits.
- The CMP must comply with all laws and rules, policies and procedures in relation to
- occupational health and safety;
- anti-discrimination, bullying and harassment;
- confidentiality, privacy and the management of personal and health information;
CMPs at TDS are expected to report knowledge of violations of the By-laws.
CMPs should report new methods of, or innovations in, treatment to professional audiences to permit evaluation and authentication before release to public news media.
Biomedical research will not be conducted at TDS
Products, devices and prostheses must have current TGA approval.
Shareholders in TDS must disclose their financial interest in TDS.
Regulation of Conduct
In accordance with the By-Laws and the Accreditation process as they may be from time to time, The Governing Body will regulate the professional conduct of accredited CMPs including the establishment of an Investigating Committee in accordance with these By-Laws.
Appeal Process
A medical practitioner who has had their request for credentialing, re-credentialing, or scope of clinical practice restricted, denied, withheld or varied from the original request has the right to appeal the decision.
The intention to appeal must be lodged within 10 working days of the decision in writing with the Governing Body. Then the appeal must be lodged within one calendar month of receiving the decision.
TDS may co-opt additional nominees to form an investigating committee that represents a range of disciplines who have the necessary skills and experience to provide informed and independent advice. This may include;
- at least one medical practitioner who practises in the field relevant to the clinical scope being reviewed
- a nominee of the relevant college, association or society
- a nominee medical practitioner of the person who is the subject of the appeal.
The Governing Body shall notify the applicant and the Investigating Committee in writing of the time and place of the Appeal Hearing.
Suspensions
The Medical Director or in their absence the Director of Nursing is authorised to act for and on behalf of the MAC in suspending Accreditation without notice until the next MAC meeting at which time ratification or review of such action can transpire.
- Refer to Medical Suspensions and Investigating Policy for details of this process.
The CMP shall;
Adopt TDS’s policies and procedures in all conduct, and comply with the National Standards of Safety and Quality in Health Services, and with all TDS Infection Prevention policies and procedures.
Practise within their scope of practice and adhere to regulatory guidelines as set by the Department of Health - Victoria.
Be responsible and accountable for the admission of their patients to TDS.
Be part of multidisciplinary collaboration between management and staff at TDS
Where the CMP calls in another doctor in consultation, the CMP must advise the Registered Nurse in Charge as to who will be responsible for patient care and the point of call following discharge.
CMP’s must notify the Medical Director within 24 hours of becoming aware of a post-operative adverse event in a patient treated at TDS within the previous 28 days. Adverse events include:
- death of a patient,
- admission to another hospital directly related to the procedure performed at TDS
- post-operative infectionCMP’s must organise bacteriological examination of all cases of post-operative infection in any patient treated at TDS
- CMP’s must notify the Medical Director and/or Director of Nursing within 24 hours of making a diagnosis of post-operative infection in a patient treated at TDS and must report results of related pathological investigations as soon as available and provide copies to TDS as soon as practicable after receipt.
- CMP’s must notify the Medical Director and/or Director of Nursing if a patient is admitted to another facility following discharge due to a decline or complication
- CMP’s must ensure that in the case of a carcinoma diagnosis the Medical Director and/or Director of Nursing must be notified soon as practicable after surgery, in line with VAED statutory requirements.
CMPs must advise the Medical Director in writing of any changes in their details i.e Contact numbers, changes of address, back up practitioner to be contacted in the event of the CMP being unavailable in urgent situations.
If the Registered Nurse in charge of TDS determines a patient is in an emergency situation, the following procedures will be adopted:-
- Every endeavour will be made to ensure that the CMP of the patient is contacted.
- TDS reserves the right to summon further help, in the interest of patient safety. This may include calling another CMP or the transfer of the patient to a suitable facility via ambulance.
- A full report will be made to the CMP as soon as practicable. In addition the doctor summoned in such an emergency situation will be requested to directly contact the patient’s CMP
CMP’s admitting patients to TDS must ensure valid consent for the intended procedure is obtained, documented and signed on a TDS approved consent form.
CMP’s are not to add extra procedures on the day of surgery, unless the patient has been fully informed and consented prior to admission and discussion held with TDS staff that time and equipment allows for proceeding.
TDS staff are to sight the consent form prior to commencement in accordance with relevant policies.
Surgery will not proceed until valid consent is sighted.
Discussion of fees with patients prior to the provision of the services:
CMP’s (or delegate) must discuss the surgical and other related fees prior to commencing treatment, ensuring that informed financial consent has been obtained.
Patients are given a 7 day cooling off period.
TDS has not attempted to establish fee schedules for its CMP’s. CMP’s are expected to make charges commensurate with what is considered reasonable in this community for this service.
Patient Management
The responsibility of a CMP includes:
- preoperative diagnosis and care
- appropriate pre-operative screening
- performance of the operation
- all related postoperative care.
- Pre admission assessments must be documented in the patients’ healthcare record and made available to TDS staff prior to admission to TDS.
During the course of a patient’s treatment at TDS concise, legible and relevant information shall be documented in the patient’s medical record
All orders for treatment of the patient shall be clearly conveyed to the nursing staff by the CMP directing such treatment
All aspects of the TDS Patient Care Record must be completed as close to the time of treatment as possible
The nursing staff and patient must be provided with clear written instructions regarding discharge of patients and follow-up arrangements.
Confidentiality Every patient’s right to privacy must be respected. The CMP should maintain the confidentiality of information from and about the patient, except such information as must be communicated for the patient’s proper care, or as is required by law.
Open Disclosure of Adverse Patient events]TDS has a policy of open disclosure for all clinical adverse events and follows the principles detailed by the Open Disclosure framework, 2013 (Australian Commission on Safety and Quality in Healthcare).
It is the responsibility of the CMP to complete the Open Disclosure Procedure as outlined in TDS policy.
All staff, including CMPs, are to undergo open disclosure training.
Antimicrobial StewardshipThe prescribing of antibiotics will be in accordance with the Australian Commission on Safety and Quality in Health Care Antimicrobial Stewardship Clinical Care Standard.
If antibiotics are prescribed or used, it must be documented including the time, route, dose, patient’s weight and indication in the TDS Patient Care Record.
Antibiotic usage will be audited periodically by TDS.
Quality and Safety
CMP’s are expected to contribute to the ongoing quality and safety of TDS by participating in the quality management program through peer review, collection of relevant clinical indicators and assistance with quality and safety activities as required. All CMPs are to follow current TDS policies and procedures, NSQHS standards, Infection Control standards and DHHS regulations.
Partnering with ConsumersPatients and their carers are to be involved in shared decision making, informed consent and all aspects of care in relation to their treatment, pre- admission and discharge planning. They must be provided with adequate written information for pre-treatment and discharge including phone numbers in case of any concerns. Patients will be asked to participate in patient experience surveys.
Open Disclosure Policy
Purpose
Open disclosure is a patient and consumer right and an essential professional requirement of healthcare delivery in Australia. It is directed and guided by The Australian Open Disclosure Framework.
Open Disclosure will be managed at Templestowe Day Surgery (TDS) through thorough clinical review and investigation of adverse events and related outcomes, with a focus on clinical risk, quality improvement and prevention of recurrence.
This policy outlines all required practices to be implemented in this instance at TDS. All TDS staff will be encouraged and supported to use the CAR system to report clinical incidents, near misses and adverse events.
Scope
This policy applies to all staff at TDS, including all credentialed medical and other practitioners.
Definitions
Adverse event: an incident that results, or could have resulted, in harm to a patient or consumer. A near miss is a type of adverse event.
Australian Open Disclosure Framework: provides a framework for health service organisations and clinicians to communicate openly with patients when health care does not go to plan.
Near miss: an incident or potential incident that was averted and did not cause harm, but had the potential to do so.
Open disclosure: an open discussion with a patient and family/carer about an incident that resulted in harm to the patient while receiving health care. The criteria of the open disclosure process include an expression of regret, and a factual explanation of what happened, the potential consequences, and the steps taken to manage the event and prevent recurrence.
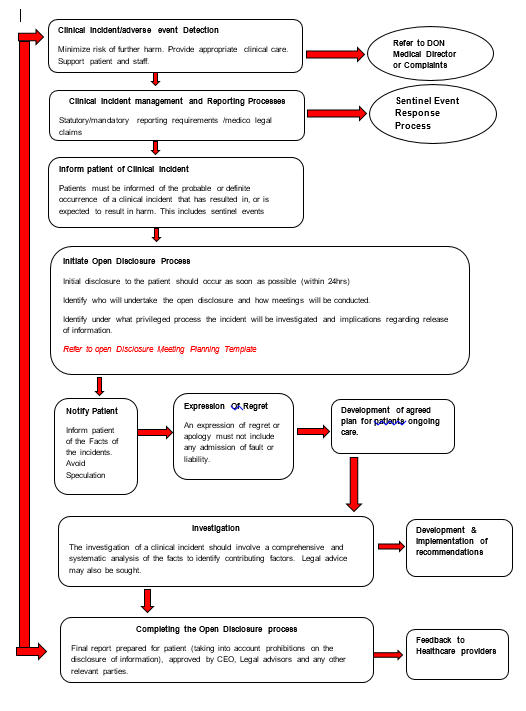
KEY ELEMENTS OF THE OPEN DISCLOSURE PROCESS (see Flowchart in Appendix A)
Patients and carers will be provided with information about what incidents and concerns are, and how to report them.
Prompt clinical care of the patient will be provided following an adverse event to prevent further harm
Staff will be supported at all times by their colleagues and TDS managers both personally (emotionally) and professionally, including through appropriate training, preparation and debrief.
Patient and clinician privacy and confidentiality must be maintained at all times.
Staff may report adverse events anonymously.
Adverse events will be raised with the senior Dr as soon as practicable following occurrence.
Adverse events will be documented using the Corrective Action Report (CAR) system on the TDS Google Drive.
The senior clinician (Dr or DON/senior Registered Nurse) on duty will assess the incident for severity of harm and level of response and document in the CAR.
The relevant professional indemnity insurers will be informed if there is a perceived risk of material, financial or reputational damage due to the incident.
Upon notification of an adverse event the senior clinician will:
- provide assistance for the reporting staff member
- acknowledge the event with the patient and family and provide an appropriate expression of regret or apology. This should include the words ‘I am sorry’ or ‘we are sorry’, but must not contain speculative statements, admission of liability or apportioning of blame. See Saying Sorry: a guide to apologising and expressing regret in open disclosure for further ideas (www.safetyandquality.gov.au/opendisclosure)
- assist staff member to commence an investigation
- determine the need for reporting to further authorities
- notify relevant staff of the incident and their need for involvement in investigation and provide ongoing support
- ensure privacy and confidentiality of patients and clinicians are observed at all times.
The patient and family must at all times be:
- Treated with empathy, respect and consideration
- Supported in a manner appropriate to their needs.
- Preparing for open disclosure
- Hold a team discussion to prepare for open disclosure
- Consider who will participate in open disclosure
- Appoint an individual to lead the open disclosure based on previous discussion with the patient, their family and carers
- Gather all the necessary information
- Identify the health service contact for the patient, their family and carers (if this is not done already)
- Negotiate with the patient, their family and carers or nominated contact person
- the formality of open disclosure required
- the time and place for open disclosure
- who should be there during open disclosure
- Provide written confirmation
- Provide a health service contact for the patient, their family and carers
- Avoid speculation and blame
- Engaging in open disclosure
- Provide the patient, their family and carers with the names and roles of all attendees, verbally and in writing
- Provide a sincere and unprompted apology or expression of regret including the words I am or we are sorry
- Clearly explain the incident, including a factual explanation about what happened in an open and honest manner. Ensure communication is appropriate to the participant’s situation, culture and level of understanding. Avoid speculation.
- Give the patient, family and carers the opportunity to tell their story, exchange views and observations about the incident and ask questions
- Encourage the patient, family and carers to describe the personal effects of the adverse event. It is important for the patient, family and carers to know their views and concerns are listened to, understood and considered.
- Agree on, record and sign an open disclosure plan
- Assure the patient, family and carers that they will be informed of further investigation findings and recommendations for system improvement
- Offer practical and emotional support to the patient, their family and carers
- Support staff members throughout the process
- Maintain good verbal and written communication throughout the open disclosure process
- Providing follow-up
- Ensure follow-up by senior clinicians where appropriate
- Agree on future care
- Share the findings of investigations and the resulting practice changes
- Offer the patient, family and carers the opportunity to discuss the process with another clinician (e.g. a general practitioner)
- ongoing support including reimbursement of out-of-pocket expenses incurred as a result of the adverse event
- assurance that any necessary follow-up care or investigation will be provided promptly and efficiently
- clarity on who will provide ongoing care resulting from the adverse event
- contact details for any relevant service they wish to access information about how to take the matter further, including any complaint processes available to them including the Victorian Health Complaints Commissioner if necessary (www.hcc.vic.gov.au/public/about-complaints or phone 1300 582 113).
- Completing the process
- Reach an agreement between the patient, their family and carers and the clinician, or provide an alternative course of action
- Provide the patient, their family and carers with final written and verbal communication, including
- how feedback will be provided on the investigation findings, by whom and in what timeframe.
- any changes made to minimise the risk of recurrence.
- Communicate the details of the adverse event, and outcomes of the open disclosure process, to other relevant clinicians
- Complete the evaluation surveys
- The event and outcome must be published on the TDS website in accordance with the Health Services (Private Hospitals and Day Procedure Centres) Regulations 2013
- Maintaining documentation
- Provide a copy provided to the patient, family and carers.
- Maintain a separate record of the open disclosure process
Staff must have training at commencement, with annual updates, in management of incidents, adverse events and the open disclosure process
All education will be documented by the DON and records maintained.
All staff must be prepared to participate in open disclosure.
Reporting and AUDIT
The complaints and Informed consent processes will be linked to the Open Disclosure Framework to ensure related incidents are collected, managed and reviewed for ongoing quality improvement and risk management.
Incidents, including open disclosure events will be tabulated and compiled on an ongoing basis by the DON.
All serious incidents and Open Disclosure events will be reported quarterly at MAC meetings to ensure appropriate follow up has occurred.
The incident management and open disclosure systems will be audited at least annually to ensure they are consistent with the Australian Open Disclosure Framework and are being implemented appropriately at TDS.
Incident data will be analysed, trends and opportunities for improvement identified.
References
Australian Commission on Safety and Quality in Health Care. Open disclosure standard. Sydney: ACSQHC; 2008.
NSQHSS Day Procedure Services Accreditation Workbook (October 2017)
Supporting Documents
Minutes of Medical Advisory Committee meetings
Minutes of Board of Management Meetings
Open Disclosure Framework http://www.safetyandquality.gov.au/wp-content/uploads/2013/03/Australian-Open-Disclosure-Framework-Feb-2014.pdf
Open Disclosure Training http://vhimsedu.health.vic.gov.au/opendisclosure/welcome.php
Open Disclosure Consumer Brochure
Health Services (Private Hospitals and Day Procedure Centres) Regulations 2013
TDS CAR Form
TDS CAR Register
Appendix A: The Open Disclosure Process
Patient Portal
This Page Is Designed to introduce all our quality controls and safety procedures to ensure the highest standards are met. Please scan the corresponding QR codes for information on our standards and to provide your feedback on your visit as a patient or a visitor
You can use the links below or the QR codes to browse the information and provide your feedback
Patient Satisfaction Survey questionnaire: https://forms.gle/VqLZ7jgfQfY9NM1ZA
Complaints and Compliments form: https://forms.gle/xqcLzxKQG5f3WQeM7
How Do We Manage our Quality and Safety procedures: https://drive.google.com/drive/folders/1BjOMCVJPvzxj-bE60_BHmq6yh6ei__c2?usp=sharing
You can use the links below or the QR codes to browse the information and provide your feedback
Patient Satisfaction Survey questionnaire: https://forms.gle/VqLZ7jgfQfY9NM1ZA
Complaints and Compliments form: https://forms.gle/xqcLzxKQG5f3WQeM7
How Do We Manage our Quality and Safety procedures: https://drive.google.com/drive/folders/1BjOMCVJPvzxj-bE60_BHmq6yh6ei__c2?usp=sharing